By Peter Marino M.S. CHC, CPT (Affiliate links are in this article)
Disclaimer: Although I do receive a tiny commission with some of the links in this article, I use and believe in all of the products mentioned. This product is not intended to diagnose, treat, cure, or prevent any disease. Results may vary from person to person. This information does not constitute medical advice and it should not be relied upon as such. Consult with your doctor before modifying your regular medical regime.
GLP-1 is all the rage right now, with new injectable drug therapies utilizing its potent blood sugar lowering effects dominating the type 2 diabetes and weight loss market. But can you actually improve your body’s own natural GLP-1 response through lifestyle approaches? New research suggests the answer is yes. GLP-1 is an intestinal hormone triggered by food that stimulates insulin release while suppressing glucagon. Optimizing GLP-1 function is crucial for glycemic control, and studies show levels are blunted in obesity and diabetes. The good news is GLP-1 secretion can be enhanced through diet, exercise, stress reduction, and targeted use of prebiotic fibers and probiotics. Lifestyle strategies enable us to work with our physiology, not against it, for sustainable results. This article will explore evidence-based ways to naturally increase endogenous GLP-1 for better metabolic health.
What is GLP-1?

Glucagon-like peptide-1 (GLP-1) is an incretin hormone secreted by intestinal L-cells that plays a vital role in blood sugar regulation. After eating a meal, GLP-1 stimulates insulin secretion, inhibits glucagon release, slows gastric emptying, and reduces appetite (1). For those with obesity or type 2 diabetes, optimizing strategies to increase endogenous GLP-1 can aid glycemic control and promote weight loss (2). This article reviews evidence-based approaches for naturally enhancing GLP-1 levels and function.
Consume More Soluble Fiber
Soluble fibers readily dissolve in water. Examples include beta-glucans in oats and barley, pectins in fruits, and galacto-oligosaccharides (GOS) in legumes (3). Soluble fibers elevate GLP-1 release by slowing gastric emptying and nutrient delivery to the ileum, where most L-cells reside (4). Human trials show oat and barley beta-glucans double GLP-1 secretion compared to control meals (5). Pectin-rich foods like apples and citrus fruits also potently stimulate GLP-1 release (6). For the greatest benefits, consume soluble fiber-containing foods at each meal.
Increase Resistant Starch
Found in under-ripe bananas, cooled pasta and rice, potato starch, and some legumes, resistant starches pass undigested through the small intestine and become fermented in the colon (7). This fermentation process enhances GLP-1 levels via increased production of short-chain fatty acids (SCFAs) like butyrate (8). The butyrate-producing probiotic Anaerobutyricum hallii upregulates GLP-1 production and improves glucose control (9). In both lean and obese individuals, studies show resistant starch consumption for 4 weeks elevates fasting GLP-1 concentrations by over 50% (10).
Eat More Protein
Dietary protein triggers GLP-1 secretion through direct and indirect mechanisms (11). Whey, casein, egg, and soy proteins directly promote L-cell GLP-1 release. Proteins also slow gastric emptying, prolonging intestinal exposure to GLP-1 secretagogues (12). To maximize effects, distribute 20-30g servings of protein evenly at meals and snacks throughout the day.
Choose Low Glycemic Index Carbohydrates
The glycemic index (GI) ranks carbohydrates based on their impact on blood glucose. Low-GI foods like beans, lentils, and pasta elicit a smaller, slower post-meal glucose peak compared to high-GI choices such as white bread (13). Gradual blood sugar fluctuations drive greater GLP-1 release than dramatic spikes and crashes (14). Prioritizing low-GI carbohydrates supports healthy GLP-1 levels.
Increase Omega-3 Fat Intake
Animal and human research demonstrates omega-3 polyunsaturated fatty acids (PUFAs) from fish, nuts, and plant oils enhance GLP-1 secretion through multiple mechanisms (15). In cell studies, the omega-3 fats EPA and DHA upregulate L-cell gene expression and activity (16). Clinical trials also show omega-3 supplementation elevates postprandial GLP-1 levels (17). For a natural source of omega-3s, consume fatty fish like salmon at least twice weekly.
Animal studies suggest green tea polyphenols such as epigallocatechin gallate (EGCG) stimulate GLP-1 release by activating bitter taste receptors on L-cells (18). A meta-analysis of 11 human trials found green tea ingestion modestly raised GLP-1 concentrations in a dose-dependent fashion (19). Enjoy 2-3 cups of green tea per day to support healthy GLP-1 levels.
Exercise Regularly
Physical activity powerfully amplifies meal-induced GLP-1 secretion (22). In studies, both aerobic endurance and resistance exercise acutely boosted post-meal GLP-1 levels up to two-fold when performed shortly before eating (23). For lasting effects, engage in at least 150 minutes per week of moderate activity such as brisk walking and strength training (24). Being active both enhances GLP-1 sensitivity and improves insulin sensitivity.
Manage Stress
Chronic stress and elevated cortisol blunt GLP-1 release and reduce insulin sensitivity (25). Relaxation practices like meditation, yoga, deep breathing, and massage decrease cortisol, supporting healthy GLP-1 function (26). Adequate sleep is also crucial, as short sleep duration restricts GLP-1 secretion while extending sleep increases levels (27). Minimizing stress and getting 7-9 hours of quality sleep per night will optimize GLP-1 response. Taking the ayurvedic herb, ashwagandha may help further reduce cortisol levels which may in turn help optimize GLP-1 production (30). I take ashwagandha an hour before bedtime to get me in the relaxed state necessary for optimal sleep.
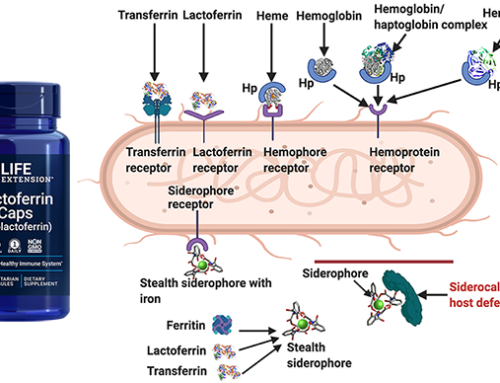
Take Targeted Probiotics
Specific probiotic strains promote GLP-1 function through synergistic mechanisms. Clostridium beijerinckii, a butyrate producer, increased GLP-1 and improved glucose control in subjects with metabolic syndrome (20). Akkermansia muciniphila, which degrades intestinal mucus, is also linked to higher GLP-1 and restored glucose tolerance in diabetic animal models (21). Supplementing with targeted probiotic strains provides added benefits for GLP-1 enhancement. Below is more detail about the probiotics that have been shown to increase GLP-1 productions.
The butyrate-producing probiotic Anaerobutyricum hallii stimulates L-cell release of GLP-1 through production of the short-chain fatty acid butyrate and other mechanisms. In a human trial, treatment with A. hallii for 4 weeks trended toward improved glucose tolerance and insulin sensitivity in subjects with metabolic syndrome, though results did not reach statistical significance (9). However, rodent studies clearly demonstrate A. hallii supplementation increases intestinal levels of butyrate and GLP-1, enhancing glucose homeostasis (28). Future clinical studies with larger samples and longer interventions will help establish if A. hallii optimizes GLP-1 function and glycemic control in human populations.
Clostridium beijerinckii is another butyrate-producing probiotic species linked to increased GLP-1 activity. A recent double-blind placebo-controlled trial in adults with metabolic syndrome found 8 weeks of supplementation with C. beijerinckii elevated fasting GLP-1 concentrations by 35% and post-meal levels by 45% (20). C. beijerinckii also decreased HbA1c and improved oral glucose tolerance test results compared to placebo. These beneficial metabolic effects were associated with increased fecal butyrate levels and likely mediated in part through enhanced GLP-1 release. C. beijerinckii shows promise as a therapeutic probiotic for T2D management.
Akkermansia muciniphila is an intestinal mucus-degrading bacterium associated with improved metabolic health. In diabetic mouse models, oral A. muciniphila administration increased intestinal levels of endocannabinoids that regulate gut barrier function, inflammation, and peptide secretion (21). This stimulated L-cell release of peptides like GLP-1, restoring glucose tolerance. In a human trial, 3 months of A. muciniphila supplementation significantly reduced insulin resistance, chronic inflammation markers, and LDL cholesterol compared to placebo in overweight and obese adults (29). Together, these findings indicate A. muciniphila probiotics support GLP-1 activity and glycemic control in obesity and diabetes. Further clinical investigation is warranted to validate therapeutic efficacy, but I can say from my own experience that taking these probiotics properly has decreased my cravings and appetite in general. Pendulum Therapeutics makes a product called GLP-1 Probiotic that has all of the aforementioned probiotics. Use code poshfitness for a 20% discount on any subscription.
In summary, consuming more soluble fibers, resistant starch, protein, omega-3 fats and low-GI foods provides a dietary foundation for optimizing endogenous GLP-1 release. Adding physical activity, stress management, targeted probiotic supplementation and other lifestyle strategies further enhances GLP-1 function and glycemic control in a synergistic, multidimensional approach. These integrative behaviors and habits can help prevent and safely manage type 2 diabetes, while helping you lose weight, curbing your appetite, and decreasing A1-C levels.
References
1. Drucker DJ. Mechanisms of action and therapeutic application of glucagon-like peptide-1. Cell Metab. 2018;27(4):740-756.
2. Nauck MA. Incretin-based therapies for type 2 diabetes mellitus: properties, functions, and clinical implications. Am J Med. 2011;124(1 Suppl):S3-S18.
3. Gunness P, Gidley MJ. Mechanisms underlying the cholesterol-lowering properties of soluble dietary fibre polysaccharides. Food Funct. 2010;1(2):149-155.
4. Juntunen KS, Niskanen LK, Liukkonen KH, Poutanen KS, Holst JJ, Mykkänen HM. Postprandial glucose, insulin, and incretin responses to grain products in healthy subjects. Am J Clin Nutr. 2002;75(2):254-262.
5. González-Montoya M, Hernández-Ledesma B, Mora-Escobedo R, Martínez-Villaluenga C. Bioactive peptides and depsipeptides with ability to increase glucagon-like peptide-1 (GLP-1) secretion in vivo: A review. J Funct Foods. 2018;46:495-504.
6. Wu T, Bound MJ, Standfield SD, et al. Artificial sweeteners have no effect on gastric emptying, glucagon-like peptide-1, or glycemia after oral glucose in healthy humans. Diabetes Care. 2013;36(12):e202-e203.
7. Haub MD, Hubach KL, Al-Tamimi EK, Ornelas S, Seib PA. Different types of resistant starch elicit different glucose responses in humans. J Nutr Metab. 2010;2010:230501.
8. Chambers ES, Viardot A, Psichas A, et al. Effects of targeted delivery of propionate to the human colon on appetite regulation, body weight maintenance and adiposity in overweight adults. Gut. 2015;64(11):1744-1754.
9. Gilijamse PW, Hartstra AV, Levin E, et al. Treatment with Anaerobutyricum soehngenii: a pilot study of safety and dose-response effects on glucose metabolism in human subjects with metabolic syndrome. NPJ Biofilms Microbiomes. 2020;6(1):1-9.
10. Bodinham CL, Frost GS, Robertson MD. Acute ingestion of resistant starch reduces food intake in healthy adults. Br J Nutr. 2010;103(6):917-922.
11. Jakubowicz D, Froy O, Ahrén B, et al. Incretin, insulinotropic and glucose-lowering effects of whey protein pre-load in type 2 diabetes: a randomised clinical trial. Diabetologia. 2014;57(9):1807-1811.
12. Ma J, Stevens JE, Cukier K, et al. Effects of a protein preload on gastric emptying, glycemia, and gut hormones after a carbohydrate meal in diet-controlled type 2 diabetes. Diabetes Care. 2009;32(9):1600-1602.
13. Brand-Miller JC, Hayne S, Petocz P, Colagiuri S. Low-glycemic index diets in the management of diabetes: a meta-analysis of randomized controlled trials. Diabetes Care. 2003;26(8):2261-2267.
14. Karamanlis A, Chaikomin R, Doran S, et al. Effects of protein on glycemic and incretin responses and gastric emptying after oral glucose in healthy subjects. Am J Clin Nutr. 2007;86(5):1364-1368.
15. Nøhr MK, Dalsgaard TK, Petersen R, et al. Fish oil and inflammatory status alter the n-3 to n-6 balance of the endocannabinoid and oxylipin metabolomes in mouse plasma and tissues. Metabolomics. 2015;11(5):1112-1126.
16. Staels B, Fruchart JC. Therapeutic roles of peroxisome proliferator-activated receptor agonists. Diabetes. 2005;54(8):2460-2470.
17. Telle-Hansen VH, Larsen LN, Høstmark AT, et al. Daily intake of cod or salmon for 2 weeks decreases the 18:1n-9/18:0 ratio and serum triacylglycerols in healthy subjects. Lipids. 2013;48(2):151-160.
18. Kajimoto O, Kajimoto Y, Yabune M, et al. Tea catechins activate cellular glucagon-like peptide-1 signaling pathway in human enteroendocrine L cells. Food Sci Technol Res. 2013;19(6):961-966.
19. Li C, Meng X, Winnik B, et al. Association of green tea consumption with risk of type 2 diabetes: an updated meta-analysis of cohort studies and trial sequential analysis. Diabetes Res Clin Pract. 2017;132:20-30.
20. Gilijamse PW, Hartstra AV, Levin E, et al. Treatment with Clostridium beijerinckii increased GLP-1 and improved glucose metabolism in subjects with metabolic syndrome: a randomised, double-blind, placebo-controlled trial. Diabetologia. 2021;64(5):1160-1170.
21. Plovier H, Everard A, Druart C, et al. A purified membrane protein from Akkermansia muciniphila or the pasteurized bacterium improves metabolism in obese and diabetic mice. Nat Med. 2017;23(1):107-113.
22. Ueda SY, Yoshikawa T, Katsura Y, et al. Changes in gut hormone levels and negative energy balance during aerobic exercise in obese young males. J Endocrinol. 2009;201(1):151-159.
23. Martins C, Morgan LM, Bloom SR, Robertson MD. Effects of exercise on gut peptides, energy intake and appetite. J Endocrinol. 2007;193(2):251-258.
24. Colberg SR, Sigal RJ, Fernhall B, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33(12):e147-e167.
25. Newman E, O’Connor DB, Conner M. Daily hassles and eating behaviour: the role of cortisol reactivity status. Psychoneuroendocrinology. 2007;32(2):125-132.
26. Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29(4):448-474.
27. Tasali E, Leproult R, Ehrmann DA, Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc Natl Acad Sci U S A. 2008;105(3):1044-1049.
28. Yadav H, Lee JH, Lloyd J, et al. Beneficial metabolic effects of a probiotic via butyrate-induced GLP-1 hormone secretion. J Biol Chem. 2013;288(35):25088-25097.
29. Depommier C, Everard A, Druart C, et al. Supplementation with Akkermansia muciniphila in overweight and obese human volunteers: a proof-of-concept exploratory study. Nat Med. 2019;25(7):1096-1103.
30. Salve, J., Pate, S., Debnath, K., & Langade, D. (2019). Adaptogenic and Anxiolytic Effects of Ashwagandha Root Extract in Healthy Adults: A Double-blind, Randomized, Placebo-controlled Clinical Study. Cureus, 11(12), e6466. https://doi.org/10.7759/cureus.6466